
Rogers’ RetrainOCD app yielding promising results, as research continues
09/20/21 02:55:pmAfter launching system-wide in April 2020, Rogers’ “RetrainOCD” app is delivering high usage rates, improved outcomes, and, in some cases, shortened stays.
“Research shows that the app enhances treatment,” says Brad Riemann, PhD, chief clinical officer. “Treatment as usual works – we’ve been doing it at Rogers for 24 years, but this makes it better and results in even more symptomatic reduction.”
Led by Dr. Riemann and the Rogers Research Center, four studies are underway to learn more and to find additional ways to innovate and expand usage.
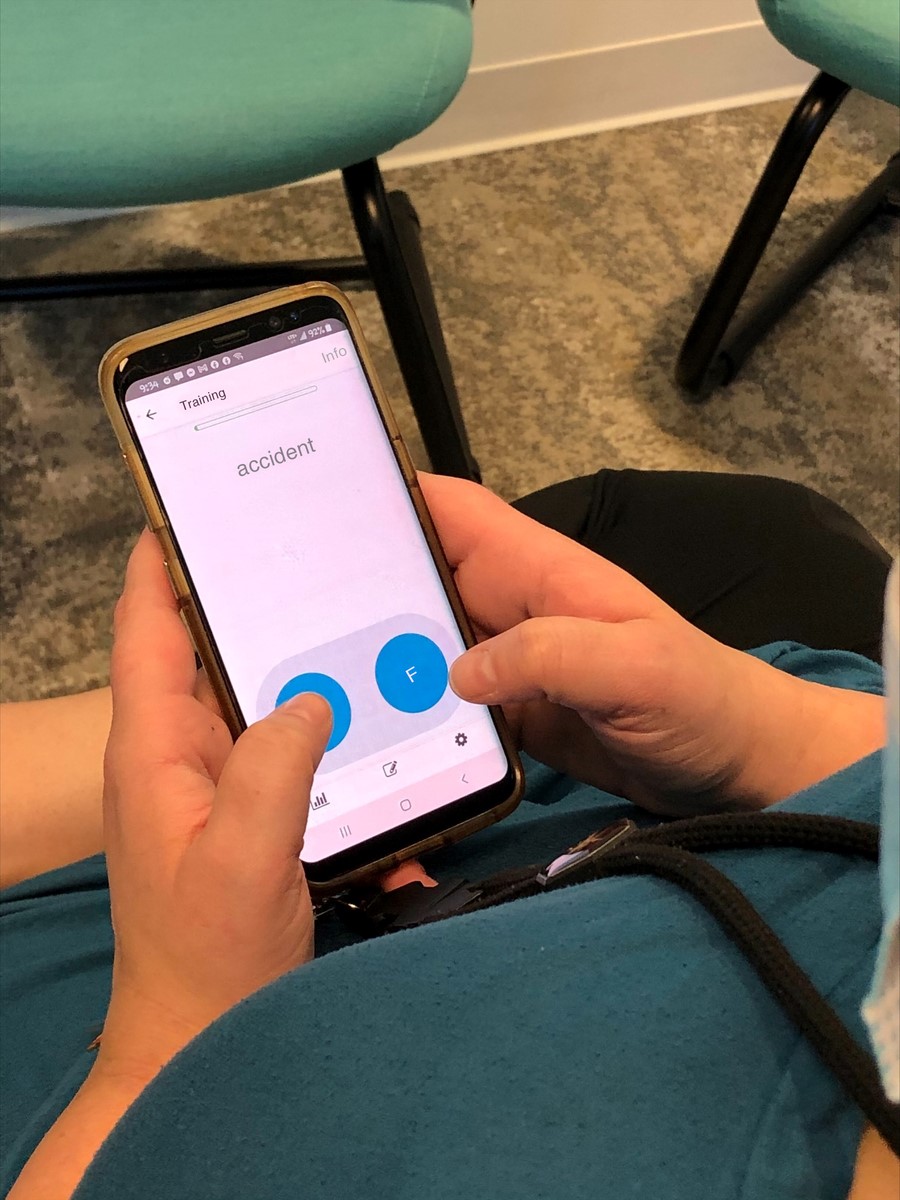
How the app works

“We don’t know if it’s getting them to shut off their radar, which is constantly scanning for threats in their environment, or if it’s getting them to disengage from the threat word faster, but it works,” Dr. Riemann says.
Dr. Riemann and his team are writing manuscripts on two recent studies: one examining the results from patients at OCD and Anxiety Adult Residential Care at Cedar Ridge and another with community members who were diagnosed with OCD but were not in treatment.
Using the Yale Brown Obsessive Compulsive Scale (Y-BOCS), patients who used the app had a significant reduction in patient-reported OCD symptoms compared to those who did not use the app. Participants in the community study also had symptom reduction by using the app only eight times over one month.
“Getting it into the hands of patients”
“Based on the preliminary research findings, we felt an obligation to spread this to our patients,” Dr. Riemann says.

As of August 2021, Rogers reached the initial goal of 60% app usage for OCD patients across the System, and seven of 20 clinics have already attained 80% usage.
While not every adult OCD patient is expected to use the app due to factors including severe dyslexia, visual impairment, sensitivity to eye movement, and the inability for some people to touch a device because of germs, the Oconomowoc partial hospitalization (PHP) and intensive outpatient programs (IOP) have achieved 100% usage for the last four months.
To promote participation, Rogers designated “app champions” at all 20 clinics and residential programs. App champions provide local technical support for staff and patients and work closely with the app support team to identify best practices for app implementation. They also have participated in the first quarterly app champion sharing session between clinics.
“There’s something powerful about people learning from their peers and sharing information with each other. The engagement between clinics has resulted in increased app usage by our patients,” says Jill Riemann, a member of the app support team and clinical research coordinator.
“We’re working closely with staff to increase patients’ confidence and compliance,” she continues. “It can be hard for them to see or feel the progress as it’s happening, so it’s important to explain why it’s worth their 10 minutes each treatment day.”
Tim Grinwald from the app support team also recently deployed Rogers-owned devices to each clinic for patients who either do not have a smartphone or struggle with application use on their personal device.
Tim has noticed the increase in usage has also coincided with the clinic device rollout.
“Having access to a reliable device takes some of the frustration away and encourages participation for patients who aren’t as comfortable with technology,” Tim says.
Next steps
A retrospective study is currently in progress to measure the impact of app use from April 2020 to August 2021. This study expands on the original residential treatment study to include PHP and IOP levels of care and will compare overall outcomes of patients who used the app versus those who did not.
Additionally, Rogers is conducting a study to determine if patients who continue to run the app for three months post-discharge will see any further improvement in symptoms or maintain their gains longer.
For now, only adults in OCD and Anxiety programs are using the app, but Dr. Riemann and Kelly Piacsek, PhD, vice president, Research, say that it could become part of treatment as usual for adolescents in the future.
In fact, Dr. Riemann was part of a 2013 study, which found that adolescent residential OCD patients had a significantly greater reduction in symptoms than those who did not receive attention retraining.
Beyond OCD and Anxiety, the app could also be used to benefit patients in other service lines such as Eating Disorder Recovery, Depression Recovery, and Trauma Recovery, but these treatment areas are still under evaluation.
The impact of Rogers Research Center
While the origins of RetrainOCD and its first published study predate the research center, the facility is helping to advance app research and development.
“The Rogers Research Center gives us the horsepower to have four active studies right now,” Dr. Riemann says. “It provides us the resources to accelerate the process and to do it at a much higher level.”
According to Dr. Piacsek, now that the research center infrastructure is in place, Rogers has the ability to do more studies and to more efficiently conduct research in areas like attention retraining, among several other priority areas.
“The app’s high rates of clinical use combined with the resources and processes within the Research Center allow us to continue to explore ways to improve app effectiveness and, ultimately, patient outcomes,” she says.





