
Rogers Research Center gearing up for contingency management study
01/18/22 03:35:pm
The study, facilitated through the Rogers Research Center, will be conducted in collaboration with Aurora Research Institute and led by Rogers principal investigator Michelle Maloney, PhD, system clinical director of Mental Health and Addiction Recovery.
“One of the things I’m excited about with this research is that Aurora and Rogers are coming together to explore how best to support patients, despite typically being seen as competitors,” Dr. Maloney says. “Collaboration is better for the patient and advances the behavioral health field. Whatever we find out, one of the takeaways is that collaboration can really benefit everyone.”
Massachusetts Institute of Technology Sloan Management School is another partner, as well as the Abdul Latif Jameel Poverty Action Lab (J-PAL), which funded the study.
Exploring the use of contingency management
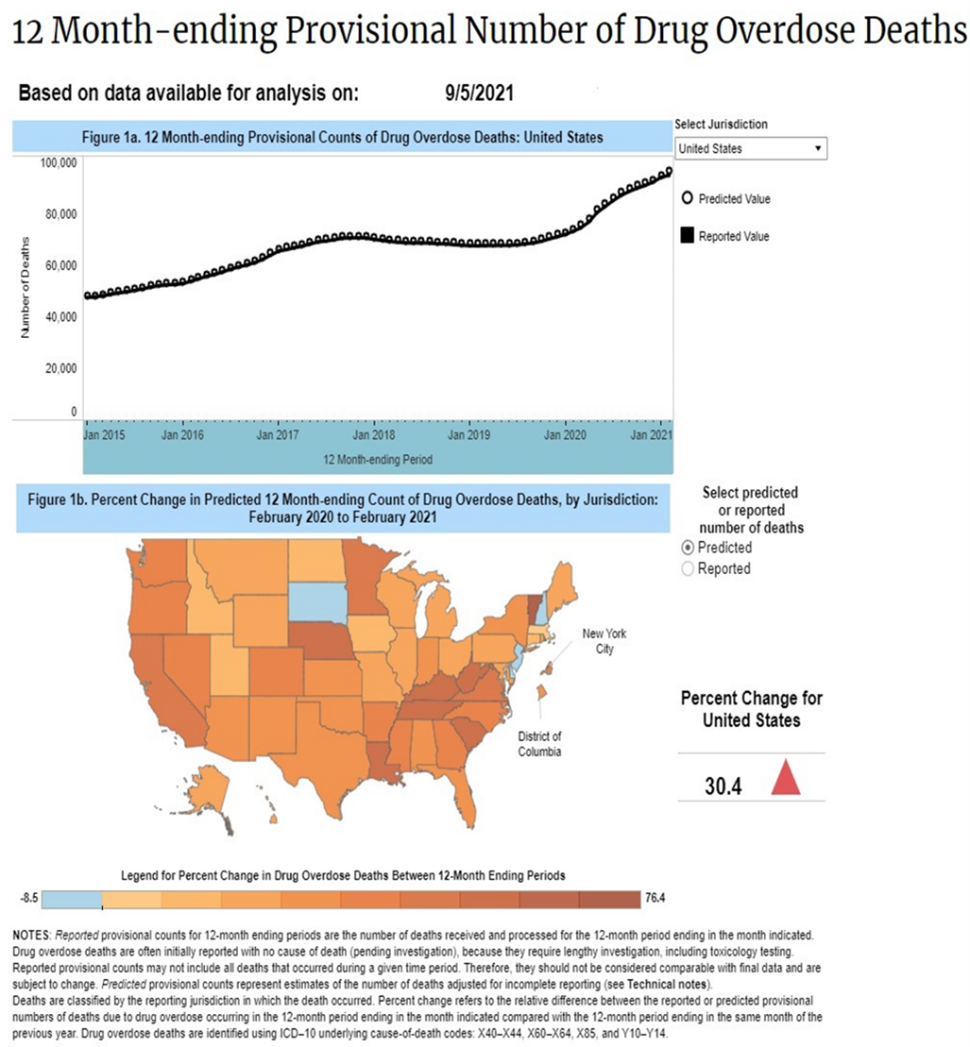
As overdose deaths are on the rise nationwide, the purpose of this study is to find out if using a contingency management smartphone app will incentivize patients with opioid or cocaine use disorders. While contingency management has been extensively studied, this research will explore what levels of incentives are the most effective for different patients.
“Contingency management is an evidence-based practice for substance use that has been around for years,” Dr. Maloney explains. “It was originally designed for stimulants, but because of the current opioid and methamphetamine crisis, it’s resurfaced to the point where the state of California is paying patients to stay in recovery.”
A type of behavioral therapy, contingency management reinforces, or rewards, people for evidence of positive behavioral change. The reinforcers typically consist of vouchers for retail goods and services or the opportunity to win prizes.
“While it can be controversial because it’s perceived as paying people money to stay in recovery, contingency management helps keep the patients focused on internal motivation versus external motivation,” Dr. Maloney says.
Few mental health professionals are familiar with these interventions, and even fewer implement contingency management in their practice. Here at Rogers, Dr. Maloney says it is used in limited capacity, but there are plans to implement it more broadly within the Mental Health and Addiction Recovery service line.
Barriers to contingency management include the stigma associated with motivating patients to recover using monetary incentives, as well as lack of available funds to provide those rewards. The positives are that it teaches new behaviors and promotes self-esteem and self-confidence. (See sidebar for more details.)
Contingency Management
-
Teaches new behaviors and promotes growth
-
Promotes self-esteem and self-confidence
-
Increases positive atmosphere and communication
-
Frequently monitors target behavior
-
Provides incentive when target behavior occurs
-
Removes incentive when target behavior does not occur
What the study entails
Researchers plan to begin recruiting study participants in February. The goal is to enroll 600 patients between Rogers and Aurora and assign them to five groups: a control group that will receive no incentives and four groups that will engage in different levels of escalation models, earning varying amounts of rewards.
The study is expected to take about nine months, including a short induction period, a three-month intervention period, and post-intervention follow-up surveys after three and six months.
The primary objective is for patients in the study to achieve a long period of continuous abstinence from non-medical opioids and cocaine, where abstinence is measured using lab-verified, in-person urine tests or video-verified saliva tests.
The study will also evaluate the number of negative saliva test results and psychotherapy appointments attended, as well as the rates of discharging from treatment before completion, relapsing, and appropriately transitioning to step-down care. Longer-term outcomes will include participant drug use at three months and six months.
“The longer someone is in recovery, the more incentives they will receive,” Dr. Maloney says. “We believe there is an upper limit on the incentives that motivate positive behavior, so we assume that once participants hit a certain level, they will plateau, and their positive behavior will be reinforced.”
To learn more about the study and contingency management, including why it works within the substance use population and the evidence behind it, tune in for Dr. Maloney’s Brownbag presentation on Friday, February 4.





